
In the ACT
Abraham Cheluget knocks on Charles’ door, and Charles welcomes him in. They sit in the living room, having an easy conversation about the challenges of keeping up the apartment, how Charles is doing, and what he needs. “I’d like to see a psychiatrist,” Charles says, and Cheluget makes a note and confirms that he’ll schedule an appointment as soon as possible. The next topic is work, and Cheluget mentions a local retail store is hiring; it’s work Charles thinks he can do and would like to try. Cheluget talks through this idea with Charles, and sets about helping Charles complete an online application.
Charles lives independently and manages his mental health challenges with support from RHD Delaware Assertive Community Treatment (ACT) team. This visit is an example of how RHD ACT teams support people living in the community — in just a few moments, in a comfort of his own home, Charles has talked through his goals, worked on some life skills, managed his daily medication and gained support in finding employment.
“Charles deserves the chance to live in his community, like everybody else,” said Cheluget, an RHD Delaware ACT case manager.
RHD supports 11 ACT programs across the country, which provide recovery-focused, multidisciplinary, intensive support for people in recovery from serious mental illness. Through regular in-home visits and coordinated assistance, RHD ACT brings together counselors, psychiatrists, registered nurses, case managers and vocational specialists to help individuals maintain employment and social relationships, live independently and manage their health. RHD ACT programs work to ensure a recovery-oriented system of care is available and prepared to carry out a full range of treatment functions wherever and whenever needed.
RHD ACT teams have a 95 percent housing retention rate, and routinely post a hospitalization rate of only 6 percent — about half the national average.
 “It’s important to work with people and see them in their environment, because you see so much more and get a better picture,” said Laura Marvel, co-director of RHD Delaware ACT. “Our ability to go to them puts people at ease; if we can make things comfortable for the person we’re supporting, they’re likely to be more open. We support and encourage independence — we don’t want to do things for people, but help them gain the capacity to do things for themselves.
“It’s important to work with people and see them in their environment, because you see so much more and get a better picture,” said Laura Marvel, co-director of RHD Delaware ACT. “Our ability to go to them puts people at ease; if we can make things comfortable for the person we’re supporting, they’re likely to be more open. We support and encourage independence — we don’t want to do things for people, but help them gain the capacity to do things for themselves.
“We really work on life skills. Healthy eating, healthy relationships, personal hygiene, everything that it takes to keep people living in the community.”
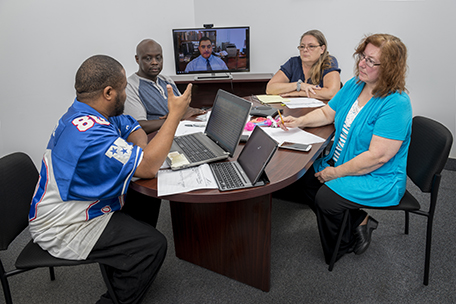
At RHD ACT in Delaware, that has involved embracing telepsychiatry. With Dr. Shelley Sellinger and Insight, one of the nation’s leading telepsychiatry providers, RHD’s ACT teams in Delaware developed a telepsychiatry program that is the first program of its kind in the nation.
Dr. Sellinger provides 32 hours of scheduled telepsychiatry services per week to RHD’s Dover program from her home office in New York. In-home sessions on an iPad work in conjunction with office visits where a telepsychiatrist is also a part of the care team.
“We were trying to be creative in working through a real shortage of available psychiatry providers,” Marvel said. “It was a challenge for us to get people regular care. With telepsychiatry, if we can’t get people in, we can take an iPad and go to them. We can use technology to make sure people get the support they need.”
Marvel and Dr. Sellinger presented the program in a peer-reviewed session at the American Telemedicine Association Annual Conference. The results have been excellent.
“I’ll admit it was weird at first, talking to a TV screen,” said David, an ACT client. “But it’s been very good. I’ve had no problems at all — if you need to talk to somebody, they’re there for you. This program has been very good. They are good people. They meet your needs; they ask you what you’re looking to accomplish and they help you meet your goals.
 “All you’ve got to do is let them know.”
“All you’ve got to do is let them know.”
ACT teams create support and treatment in a community setting, working to enable individuals with mental illness to live in their community to the fullest extent and to achieve recovery — at a far lower cost to the community than repeated extended hospital stays.
“RHD wraps services and supports around the individual, and responds quickly in times of crisis to help the participant remain in their community, and not return to an institutional setting,” said Gina Hiler, RHD Midwest Regional Director, who oversees two ACT teams in Iowa. “The participant is always the central and driving force of the services and supports we deliver each day.
“We support each participant in building their life in their chosen community; a life defined by the participant and supported by each member of RHD’s staff.”


